How to Choose Ointment for Bedsore? Understanding Causes and Prevention for Bedsores
When caring for elderly family members who are bedridden or wheelchair-bound at home, it is important to be aware of common bedsore issues. Since they may have difficulty changing their positions on their own, the doctor will not only advise us to regularly turn and reposition our family members but also pay special attention to common bedsore problems.
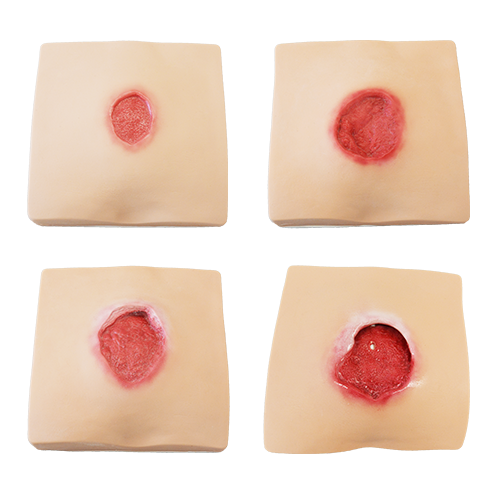
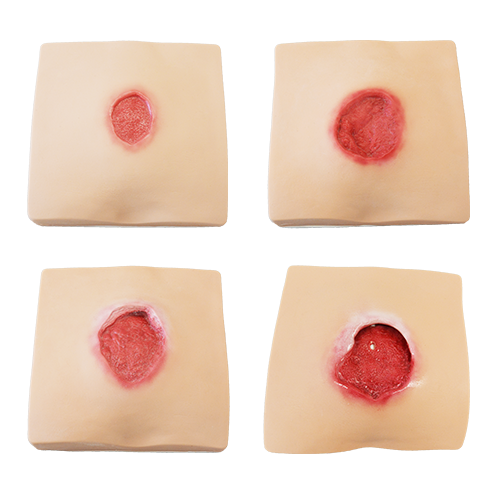
Bedsores, also known as pressure sores, are mostly caused by a combination of factors such as decreased health and mobility in patients who must maintain a fixed position for an extended period. This constant external pressure on the body and skin hampers proper blood circulation in the affected areas, resulting in skin redness, broken skins, and other forms of damage.
Then, which parts of the body are prone to bedsores? And what are the potential complications associated with pressure sores? In the following discussion, we will introduce you to the symptoms of bedsores and share preventive measures as well as key points to consider when selecting topical creams. These will help effectively alleviate discomfort and restore the skin to a comfortable state.
Where are the common areas on the body for the occurrence of p bedsores? Let’s understand the susceptible areas and populations prone to developing bedsores.
The main factors contributing to the development of bedsores are excessive pressure and friction. In clinical settings, individuals who lack the ability to change their body positions are more susceptible to bed sore symptoms. This includes bedridden patients, elderly individuals who spend prolonged periods in wheelchairs, and those with chronic illnesses. These populations are particularly prone to developing bedsores.
The common sites for the occurrence of pressure sores are typically areas where the body or bones have prominent protrusions, such as:
Hips
Heels
Elbows
Shoulders
Ears
The aforementioned areas are prone to excessive pressure and friction due to prolonged sitting or lying, making them susceptible to the development of bedsores. Therefore, special attention is required when caring for these skin areas.
What are the Causes for Bedsores? Understanding Three Major Factors Leading to Bedsores
1. Constant Pressure on Areas of the Body
Bedsores are a type of chronic wound that occurs primarily due to prolonged pressure on a specific area of the body without regular position changes to relieve the pressure. This prolonged pressure impedes blood circulation, and if the affected area extends beyond the superficial layers of the skin, it can result in broken skins, open wounds, and other related conditions. As the wound continues to expand, it develops into a bedsore.
2. Skins Frequently Exposed to Moisture
If the skin of a bedridden patient is frequently exposed to a moist environment, such as when the bed sheets become wet after urination or defecation and are not promptly cleaned and changed, or if diapers are not regularly replaced, these conditions can easily lead to skin irritation and poor ventilation. This, in turn, can contribute to the development and worsening of bedsores.
3. Poor Nutrition
Level of nutrition is also one of the factors that can contribute to the development of bedsores. If a patient experiences long-term malnutrition, it not only leads to weight loss and loss of subcutaneous fat, but also makes bony prominences more pronounced. This increases the vulnerability of those areas to the occurrence of bedsores.
What Complications Can be Caused by Bedsores? Three Most Commonly Occurring Symptoms
1. Infections in bones and joints
If bedsores occur near joints or bony areas and persist despite long-term treatment, it can lead to bacterial infection. This can potentially result in conditions such as arthritis or osteomyelitis. In addition to causing a decline in joint function, these complications can make the treatment of bedsores more challenging.
2. Cellulitis
Bedsores can cause the skin to appear red, swollen, hot, and painful. Depending on the severity of the pressure ulcer, it can result in open, non-healing wounds. When the wounds are not properly cared for and treated with ointments, the likelihood of developing cellulitis as a complication increases. Additionally, some patients may have nerve damage or reduced sensitivity to pain, requiring extra attention from caregivers to avoid missing the optimal treatment window.
3. Sepsis
If bedsores occur, it is recommended to seek medical advice ASAP and actively follow the instructions of a healthcare professional for topical medication or surgical interventions. Failure to receive proper treatment can worsen the condition and lead to complications such as sepsis, which can be life-threatening.
Prevention and Treatment of Bedsores: Improve the Environment, Regularly Reposition to Relieve Pressure, and Diligently Change Topical Medication
1. Regularly changing positions to relieve pressure
For patients who are seated or bedridden for extended periods, preventing bedsores involves more than just assisting them in changing positions and turning over every two hours to alleviate pressure and promote blood circulation. Supporting the patient with pillows and pressure-relieving mattresses can also be used as aids to prevent the development of bedsores. Additionally, while assisting with position changes, it is essential to observe the condition of the patient’s skin for any signs of bedsores. Early detection allows for timely treatment.
2. Maintaining balanced nutrition and clean and dry environment
Patients with bedsores need to ensure an adequate intake of protein, calories, vitamins, and other nutrients in their diet. Maintaining balanced nutrition is also one of the ways to prevent bedsores. Regularly washing bed sheets, keeping them smooth and dry, and selecting softer and more comfortable clothing materials for patients can reduce friction and help lower the risk of developing bedsores.
3. Using ointments or gels for bedsore treatments and diligently re-applying the dressing
When treating and caring for bedsores, it is recommended for family members to learn the proper methods. Regularly changing the dressing is important. During dressing changes, the wound should be cleaned with saline solution, and the prescribed ointment should be applied as directed by the physician. The wound should then be covered with sterile gauze to ensure its safe protection, allowing for prompt improvement of discomfort.
How to Choose Ointments or Gels for Bedsore Treatment? Follow Physician’s Assessment and Choose the Proper Medications
Based on the above information, you should have a better understanding of how to care for bedsores properly. When it comes to selecting bed sore ointments or gels for wound management, there are several factors to consider:
It is advisable to follow the prescription provided by your doctor for bedsore ointments or gels, or wound cleansing gels, to aid in wound healing. Additionally, these products typically have a high water content and a refreshing texture, which can gently remove dead skin cells and promote exfoliation.
Before the formation of bedsores, we can use products that have soothing effects on the skin as means of preventive care. Therefore, we would like to recommend the versatile healing product, “Cyan Reishi Advanced Repair Gel” from Sheng Yuan Herbs. It is formulated with gentle herbal ingredients, including the mild Chinese herb “Cyan Reishi” and the essence of GMI protein extracted from ganoderma microsporum. With its natural and safe ingredients, “Cyan Reishi Advanced Repair Gel” is designed to address various skin issues effectively.
If wounds have been developed due to bedsores, in addition to following the doctor’s instructions to use bedsore ointments or gels, you can also complement with “Cyan Reishi Advanced Repair Gel” full of moisturizing texture. The natural ingredient, GMI protein, in “Cyan Reishi Advanced Repair Gel” can greatly help repair damaged skins.
“Cyan Reishi Advanced Repair Gel” is a versatile gel that every household should have at home. It can be applied to areas prone to bedsores to enhance skin protection, alleviate dry skin problems, and address acute skin issues. It provides comprehensive repair that gives you a sense of reassurance and peace of mind.
Whether it is the patients themselves who are greatly affected by bedsores or the caregivers, it is crucial to have a clear understanding of the causes of bedsores and to rigorously implement preventive and treatment measures. Only by doing so can we expedite the recovery, meaningfully improve the situation, and say goodbye to the troubles caused by bedsores.




